Clarifi®
Clarifi makes microvascular assessment simple.
Clarifi Imaging System is the first non-contact, noninvasive microvascular assessment tool that uses a proprietary optical imaging technique — spatial frequency domain imaging (SFDI) — to measure tissue oxygenation and perfusion at the point-of-care in seconds.
Measure what matters!
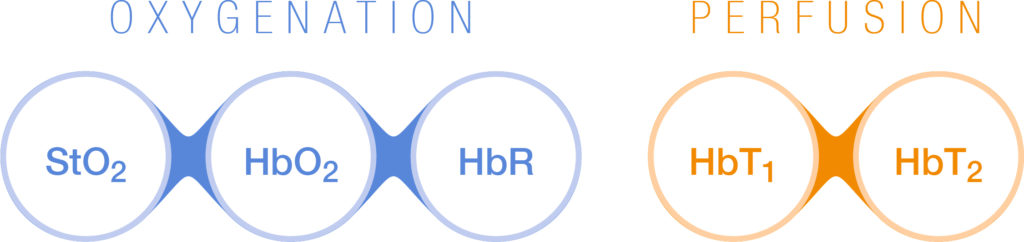
Clarifi quantifies and maps five hemoglobin biomarkers of oxygenation and perfusion. These biomarkers help clinicians identify problems, manage patients, and personalize treatment to reduce ulcers and amputations.
LAMP
Limb Assessment, Management, & Preservation solution seamlessly fits into your existing workflow
- Assess patients at the point-of-care using advanced microvascular imaging with Clarifi®.
- Manage patient care efficiently between caregivers with the ability to store and share patient data securely with Modulim Cloud.
- Preserve patient’s limbs with coordinated multidisciplinary care.
Modulim Cloud
Our HIPAA compliant Modulim Cloud creates a scalable infrastructure to allow for easy access to imaging and provides a backbone for patient data insights.
Automatic secure storage, indexing, and archiving of patient data
Curated timelines of patient progress
HIPAA compliant

Magnifi Software
- Tailored worklist shows you the data you need to see when you need to see it
- Remotely disposition patient care and follow up
- Share data with colleagues for care collaboration or second opinion
Data Insights - Patients
Innovative technology designed to aide clinicians in diagnostics, care coordination, and patient management
Assess patients at the point of care using tissue health biomarkers to help risk stratify, support care pathway decisions, and follow up frequency
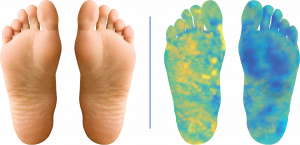
Physical exam showed no pathology. SFDI showed asymmetry, potential compromised circulation in left foot. Further vascular consultation may be needed.**
**High resolution recreations of data.
Manage patients with real time guidance by assessing the responsiveness to therapeutic interventions (e.g. targeted offloading, debridement, HBOT, stent patency, etc.)
Reduced perfusion in periwound area identified. Further intervention (e.g. debridement) may be needed to aid in healing.**
**High resolution recreations of data.
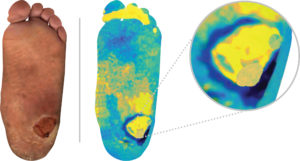
Identify focal (pre-ulcer) and systemic circulatory issues sooner allowing earlier intervention
Physical exam showed no pathology. SFDI showed focal area of compromised circulation at second metatarsal head. No intervention performed, 3 months later patient returns with ulceration (Mazhar et al., 2019).**
**High resolution recreations of data.

Data Insights – Population
Microvascular insights, data analytics, and clinical dashboards help clinicians guide care
Microvascular insights empower clinicians to manage patients with potential circulatory compromise
Other Clinical Applications + Research
SFDI can help providers with clinical insights like these:
Poor peripheral circulation in diabetes patients accelerates silent vascular changes and can lead to a diabetic foot ulcer (DFU) and Peripheral Arterial Disease (PAD). The end result for the patient is often an amputation. DFUs are common (34% of diabetes patients get an ulcer in their lifetime), costly, and debilitating (Armstrong et al., 2017). Unfortunately, PAD is underdiagnosed due to a lack of noninvasive testing. To facilitate targeted intervention before an amputation is needed, our technology measures peripheral perfusion and allows clinicians to better manage their patients’ complications.
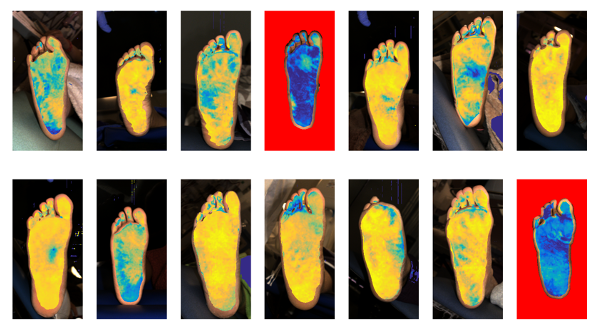
Recent publications show:
SFDI was used to identify unique signatures of compromised circulation in diabetes and PAD patients (Weinkauf et al., 2019).
SFDI was used to identify high risk patients in a larger population with the goal of risk stratification (Lee et al., 2020).
SFDI was used to differentiate the etiology (neuropathic vs. neuro-ischemic) of DFUs (Murphy et al., 2020).
SFDI Was used to stratify severity of microvascular disease (Jett et al., 2021).
SFDI was used to differentiate the etiology (neuropathic vs. neuro-ischemic) of DFUs (Murphy et al., 2020).
Immobile patients suffer from constant pressure on specific areas, resulting in ulcers that often cause pain and are difficult to heal. Pressure ulcers (or decubitus ulcers) are persistent and costly problems in hospitals, nursinghomes, and long-term care facilities. The mitigation strategy often involves constant rotation of patients, which uses the time and resources of care providers. Modulim’s SFDI technology can help clinicians monitor circulation changes that precede ulcers and allow caregivers to intervene proactively. If an ulcer has already formed, SFDI technology can help clinicians track and document the impact of treatment attempts. A recent publication demonstrated how SFDI was used as a tool for skin assessment in subjects at risk for pressure ulcers (Yafi et al. 2017).
Proper oxygenation and perfusion are critical for successful reconstructive flap procedures following mastectomies or other surgeries with pedicle flaps or free tissue transfer flaps. Although there are different ways to measure perfusion, the current standard of care relies on the subjective evaluation of tissue discoloration and temperature. SFDI provides clinicians a wide-field distribution of perfusion without the use of contrast agents. This information can enable clinicians to perform preoperative planning, intra-operative validation of successful attachment, and post-operative monitoring. A publication from 2013 showed SFDI being used for the assessment of flaps in mastectomy procedures (Gioux et al., 2013).
Treatment of burns depends on an accurate diagnosis of a wound’s severity. Unfortunately, even experts incorrectly diagnose partial thickness burns a third of the time because evaluation is based on visual inspection of wound coloring, tissue necrosis, burn surface area, and edema.
Modulim’s SFDI technology can assess the structure and function of tissue in burn areas quantitatively. Recent peer-reviewed studies have shown:
SFDI results correlate to current gold standard histology measurements of burn depth in pre-clinical models (Mazhar et al., 2014).
SFDI as a way to assess burn depth clinically (Ponticorvo et al., 2020).